Sperm Regeneration Time: Urologist Insights
Understanding male reproductive biology is essential for anyone concerned about fertility, health decisions, or lifestyle changes. One of the most frequently asked questions in urology clinics is: how long does it take for sperm to regenerate? This comprehensive guide explores the complete spermatogenesis cycle, factors that influence regeneration time, and practical insights from medical professionals.
The process of sperm production, known as spermatogenesis, is a fascinating biological mechanism that occurs continuously throughout a man’s adult life. Unlike the female reproductive system, which releases a limited number of eggs, the male body produces millions of new sperm cells daily. This remarkable regenerative capacity depends on several interconnected biological processes and can be affected by various health and lifestyle factors.

Understanding Spermatogenesis Basics
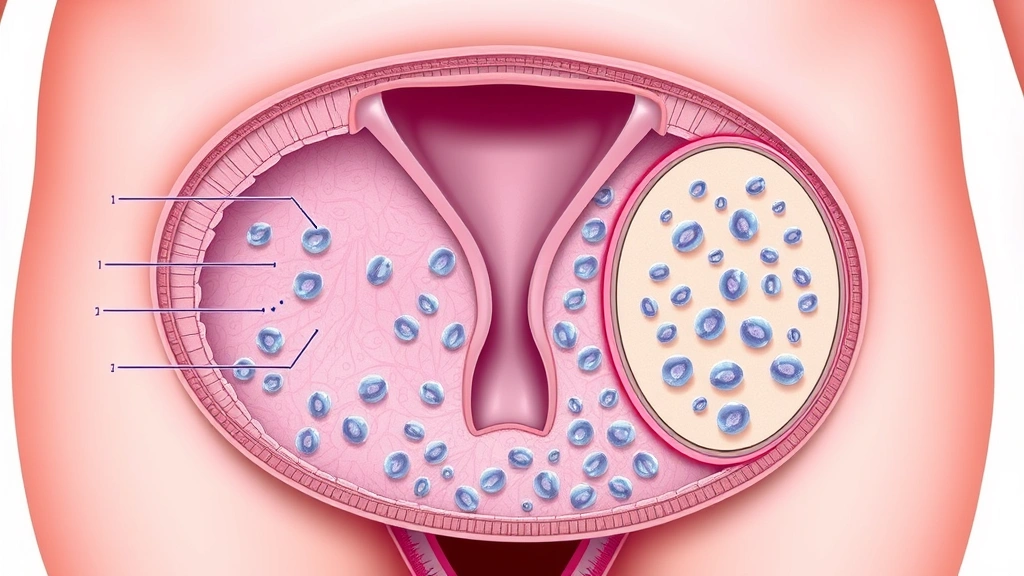
Spermatogenesis is the biological process by which mature sperm cells develop from germ cells in the seminiferous tubules of the testes. This process begins at puberty and continues throughout a man’s lifetime, though sperm production may decline with age. The journey from a single germ cell to a mature, motile sperm cell is complex and involves multiple developmental stages.
The male reproductive system produces approximately 1,500 sperm per second, which translates to roughly 130 million sperm daily. This extraordinary production rate ensures a continuous supply of viable reproductive cells. The process occurs within the testes, specifically in structures called seminiferous tubules, which are lined with specialized cells that support and nurture developing sperm.
The primary hormone driving this process is testosterone, produced by Leydig cells within the testes. Additionally, follicle-stimulating hormone (FSH) from the pituitary gland plays a crucial role in regulating spermatogenesis. Understanding these hormonal interactions helps explain why certain medical conditions or medications can significantly impact sperm regeneration.

The Complete Sperm Regeneration Cycle
The complete spermatogenesis cycle typically takes approximately 74 days from start to finish, though this timeline can vary between individuals ranging from 64 to 84 days. This extended timeline is significantly longer than many people initially expect, which has important implications for fertility planning and recovery from various reproductive health interventions.
The spermatogenesis process divides into three main phases: mitotic proliferation, meiosis, and spermiogenesis. During the mitotic proliferation phase, spermatogonial stem cells divide and multiply, creating the pool of cells that will eventually become sperm. This phase establishes the foundation for all subsequent development and requires proper nutritional and hormonal support.
The meiotic phase is where genetic material is halved, creating cells with half the chromosomes of the original cell. This is essential for sexual reproduction, as the sperm will combine with an egg to restore the full chromosome count. This phase is particularly sensitive to environmental stressors and toxic exposures, making it a critical period for maintaining sperm health.
Spermiogenesis is the final transformation phase where cells develop the characteristic sperm structure, including the head containing genetic material, the midpiece rich in mitochondria for energy production, and the tail for motility. Once this phase completes, mature sperm move to the epididymis for storage and further maturation, where they can remain viable for several weeks.
It’s important to note that while the average cycle is 74 days, the timeline for any individual sperm from initial development to ejaculation typically ranges from 74 to 90 days when accounting for epididymal storage time. This means that improvements in health or lifestyle changes may not show results in semen analysis for at least two to three months.
Factors Affecting Sperm Regeneration Time
Several biological and environmental factors can influence how quickly sperm regenerate and the quality of newly produced sperm. Age is a significant factor, with men typically experiencing peak sperm production in their twenties and thirties, gradually declining thereafter. However, unlike female fertility, male fertility generally continues throughout life, though with decreasing efficiency.
Temperature plays a critical role in sperm production. The testes maintain a temperature approximately 2-3 degrees Celsius below normal body temperature, which is optimal for spermatogenesis. Activities that increase testicular temperature, such as prolonged sitting, tight clothing, frequent hot baths, or regular sauna use, can temporarily reduce sperm production and motility. Interestingly, when you understand how long does it take for spackle to dry, you gain appreciation for biological processes that similarly require specific conditions and patience.
Nutritional status significantly impacts sperm regeneration. Adequate intake of zinc, selenium, vitamin C, vitamin E, and folate is essential for healthy sperm production. Zinc deficiency is particularly concerning, as this mineral is crucial for testosterone production and sperm cell development. Antioxidant nutrients help protect developing sperm from oxidative stress, which can damage DNA and reduce fertility.
Body weight and composition affect hormonal balance and sperm health. Both obesity and extreme leanness can disrupt testosterone production and reduce sperm count and motility. Maintaining a healthy weight through balanced nutrition and regular exercise supports optimal reproductive function.
Stress levels impact fertility through hormonal pathways. Chronic stress elevates cortisol, which can suppress testosterone production and interfere with spermatogenesis. Managing stress through exercise, meditation, adequate sleep, and social support becomes increasingly important for men concerned about fertility.
Health Conditions and Medications
Various medical conditions can affect sperm regeneration time and quality. Diabetes, particularly when poorly controlled, can impair spermatogenesis and reduce sperm motility. Thyroid disorders can disrupt the hormonal balance necessary for healthy sperm production. Infections, particularly sexually transmitted infections or prostate infections, can temporarily or permanently affect sperm production depending on severity and treatment.
Many medications impact sperm production as a side effect. Certain antidepressants, antipsychotics, and anti-hypertensive medications can reduce sperm count or motility. Chemotherapy drugs used in cancer treatment can cause temporary or permanent damage to spermatogenesis, though fertility preservation options are increasingly available. Even common pain medications like ibuprofen, when used chronically, may negatively affect fertility.
Varicoceles, which are enlarged veins in the scrotum, affect approximately 15% of men and can significantly impair sperm production by increasing testicular temperature. Surgical correction of varicoceles often improves sperm parameters, though recovery may take several months. Similarly, other urological conditions like testicular torsion or undescended testicles during development can permanently affect sperm production capacity.
Hormonal imbalances, including low testosterone or high prolactin levels, require medical evaluation and treatment. These conditions may be addressed through lifestyle modifications, medications, or in some cases, hormone replacement therapy under medical supervision. The key is obtaining proper diagnosis through comprehensive medical evaluation rather than self-diagnosis.
Lifestyle Modifications for Optimal Sperm Health
Men seeking to optimize sperm regeneration should implement comprehensive lifestyle modifications. Regular exercise, particularly moderate-intensity aerobic activity, improves cardiovascular health, hormone production, and sperm parameters. However, excessive endurance exercise or anabolic steroid use for athletic performance can paradoxically reduce sperm production.
Dietary improvements focusing on whole foods, adequate protein, healthy fats, and abundant fruits and vegetables support optimal sperm production. The Mediterranean diet pattern has shown particular benefits for male fertility in research studies. Limiting processed foods, refined sugars, and excessive alcohol consumption helps maintain hormonal balance and reduce inflammation.
Sleep quality significantly impacts reproductive health. During deep sleep, testosterone production peaks, and growth hormone supports cellular regeneration. Men should aim for 7-9 hours of consistent, quality sleep nightly. Sleep apnea, a common condition that disrupts sleep quality, has been associated with reduced sperm count and motility, making diagnosis and treatment important.
Smoking cessation provides substantial benefits for fertility. Smoking reduces sperm count, motility, and morphology while increasing DNA damage in sperm. Former smokers typically see improvements in sperm parameters within 3-6 months of quitting, though the timeline aligns with the spermatogenesis cycle discussed earlier.
Limiting alcohol consumption to moderate levels (no more than 2-3 drinks daily) protects sperm health. Heavy alcohol use can suppress testosterone production and impair spermatogenesis. Similarly, recreational drug use, particularly marijuana and cocaine, negatively affects sperm production and should be avoided.
Environmental toxin exposure deserves consideration. Pesticides, heavy metals, and certain industrial chemicals can impair spermatogenesis. Men in occupational settings with potential chemical exposure should use appropriate protective equipment and seek workplace safety measures. Just as understanding how long does it take for polyurethane to dry requires attention to environmental conditions, sperm health depends on environmental protection.
Timeline for Recovery After Vasectomy
Men who have undergone vasectomy and subsequently desire vasectomy reversal often ask about sperm regeneration in this context. Following vasectomy reversal surgery, spermatogenesis continues uninterrupted in the testes, but the key question concerns how long until sperm appear in ejaculate after the vas deferens is surgically reconnected.
The timeline for sperm reappearance after vasectomy reversal varies considerably. Some men may have sperm in their ejaculate within weeks, while others may require 6-12 months or longer. This variation depends on factors including time since original vasectomy, surgical technique, surgeon experience, and individual healing capacity.
Post-reversal semen analysis should not be performed before 8-12 weeks, as this allows adequate time for sperm to travel through the reconnected vas deferens. Early testing before this period may yield false negatives, causing unnecessary concern. Repeat testing at 3-4 month intervals may be necessary to establish whether sperm production and transport are successful.
Motility of sperm present after vasectomy reversal may initially be lower than baseline, but typically improves over subsequent months as spermatogenesis and transport mechanisms normalize. Fertility outcomes improve over the first 2-3 years post-reversal, suggesting ongoing improvements in sperm quality during this extended period.
Men considering vasectomy reversal should understand that while the surgery itself may be successful in reconnecting the vas deferens, achieving natural conception may still require time or may not occur naturally in all cases. Consultation with a reproductive urologist provides individualized guidance based on specific circumstances.
FAQ
How long does it take for sperm to fully regenerate?
Complete spermatogenesis typically takes 74 days on average, with a normal range of 64-84 days. When accounting for epididymal storage and maturation, the total timeline from initial development to ejaculation is usually 74-90 days. This means that lifestyle changes or medical treatments require at least 2-3 months to show measurable improvements in semen analysis.
Can sperm regenerate faster in younger men?
While younger men generally have more efficient spermatogenesis, the timeline of approximately 74 days remains relatively consistent across age groups. However, younger men typically produce higher quality sperm with better motility and morphology. Older men may experience slower recovery from insults to spermatogenesis and may have lower baseline sperm parameters.
Does frequent ejaculation affect sperm regeneration?
Frequent ejaculation does not impair sperm regeneration capacity. The testes continuously produce new sperm, and regular ejaculation does not deplete this supply. However, very frequent ejaculation (multiple times daily) may temporarily reduce sperm count per ejaculate, though sperm production itself continues normally. Men attempting conception may benefit from spacing intercourse every 2-3 days to optimize sperm count per ejaculation.
What supplements improve sperm regeneration?
Research supports supplementation with certain nutrients including zinc (25-30mg daily), selenium (200mcg daily), vitamin C (1000mg daily), vitamin E (400-600 IU daily), and CoQ10 (200-300mg daily). However, supplements should complement, not replace, a healthy diet and lifestyle. Excessive supplementation can be counterproductive, and men should consult healthcare providers before starting supplement regimens.
How long after quitting smoking does sperm quality improve?
Sperm quality typically begins improving within 3-6 months of smoking cessation, aligning with the spermatogenesis timeline. However, some improvements in motility and morphology may become apparent sooner. Complete recovery of sperm parameters to baseline may take 6-12 months depending on smoking duration and intensity.
Can stress affect sperm regeneration time?
Chronic stress can impair sperm production quality and potentially slow regeneration through elevated cortisol suppressing testosterone. However, stress typically affects sperm quality more than the actual 74-day regeneration timeline. Stress management through exercise, meditation, and adequate sleep supports optimal reproductive function.
Is sperm regeneration affected by age?
The basic timeline of spermatogenesis remains relatively constant across ages, but older men experience declining sperm production, motility, and morphology. Recovery from health insults or improvements from lifestyle changes may take longer in older men. Additionally, sperm DNA fragmentation increases with age, potentially affecting fertility outcomes.
